Researchers at Massachusetts General Hospital (MGH) have identified a potential mechanism by which tobacco smoking drives a type of white blood cell known as monocytes to the lung where they can increase the risk of active tuberculosis (TB).
In a recent study published in Science Translational Medicine, the team also described how the intracellular growth of Mycobacterium tuberculosis (Mtb), the causative agent of TB, could be inhibited through anti-inflammatory small molecule drugs, some of which are already approved for human use.
“Smoking is one of the strongest risk factors for TB acquisition and death, and our study suggests a model in which smoking leads to the recruitment of immature inflammatory monocytes to the lung, where they accelerate the growth of the bacterium that causes tuberculosis,” says Doug Kwon, MD, Ph.D., senior author of the study and director of clinical operations at the Ragon Institute of MGH, MIT, and Harvard.
“Our work defines how smoking may lead to increased susceptibility to TB and identifies therapies to potentially reduce the burden of TB on those who do smoke,” adds Benjamin Medoff, MD, a co-senior author on the study.
Tuberculosis affects more than 20% of the global population, and is responsible for the deaths of 1.3 million people every year.
The majority of people infected with Mtb develop a subclinical latent form of the disease, with about 5% to 10% progressing to active TB when the immune system becomes overwhelmed and is no longer able to control the infection.
In the United States, 8,331 cases of TB were reported in 2022, and up to 13 million people in the U.S. are believed to be living with latent TB infection, according to the Centers for Disease Control and Prevention.
While smoking has long been considered a strong risk factor for active TB, the specific mechanisms underlying the relationship have remained poorly understood. Globally, 1.3 billion people smoke tobacco, resulting in an estimated 10% to 20% of all active TB cases.
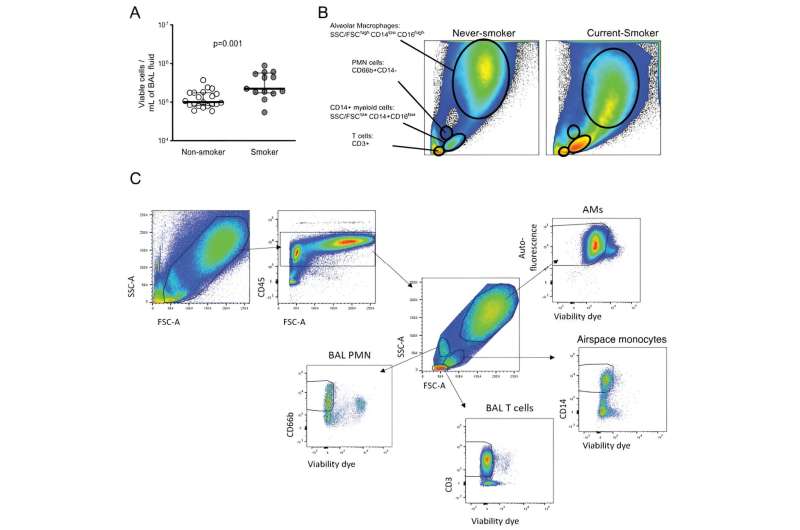
Using single-cell RNA sequencing, flow cytometry, and blood and lung specimens from smokers and non-smokers, MGH researchers performed the most detailed study to date of how smoking perturbs the composition and state of the lung microenvironment to promote increased Mtb growth.
“In this interdisciplinary and human immunology study, we demonstrated that blood and lung monocytes from smokers produce elevated inflammatory responses following exposure to Mtb, and that immature monocytes support increased rates of Mtb intracellular growth relative to developmentally mature versions of those cells,” explains Bjorn Corleis, Ph.D., a former infectious disease postdoctoral fellow at the Ragon Institute of MGH, MIT, and Harvard, and co-lead author of the study.
“This biological understanding supports the conclusion that tobacco smoking primes the pro-inflammatory lung environment and malfunctioning immune response.”
Just as importantly, researchers showed that treatment of monocytes with anti-inflammatory drugs can inhibit intracellular Mtb growth.
One of those small molecule agents is dexamethasone, a corticosteroid that has already been approved to reduce inflammation and increase survival in patients with tuberculosis-associated immune reconstitution inflammatory syndrome (TB-IRIS) and TB-associated meningitis.
Another agent found to act as an anti-inflammatory mediator against TB is SP600125, a small molecule kinase inhibitor used to treat various types of cancer.
“Further research is needed to explore the effects of tobacco smoke on lung immune cells and, more specifically, how we can reverse the effects of smoking,” reports Medoff.
“By providing biological insights into the mechanism by which smoking increases Mtb growth, our team has not only advanced the science but opened the door to potential new treatments that could help millions of people around the world battling this deadly infection.”
More information:
Björn Corleis et al, Tobacco smoke exposure recruits inflammatory airspace monocytes that establish permissive lung niches for Mycobacterium tuberculosis, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.adg3451
Journal information:
Science Translational Medicine
Source: Read Full Article