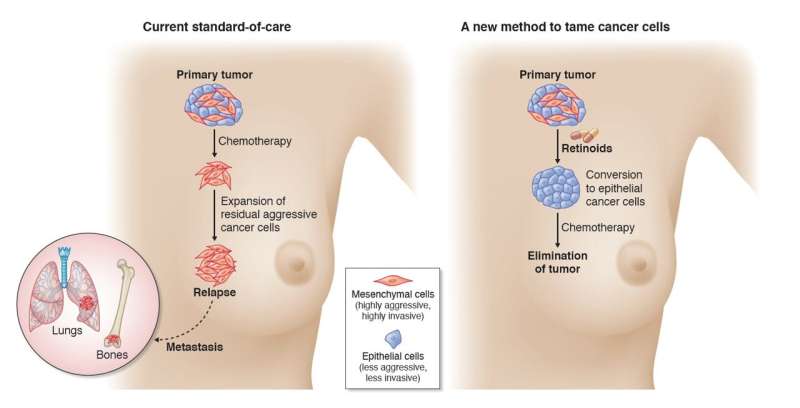
A team of clinicians and scientists from the National Cancer Centre Singapore (NCCS), Singapore General Hospital (SGH) and A*STAR’s Genome Institute of Singapore (GIS) has identified a novel method to treat triple-negative breast cancer (TNBC). They discovered that cancer cells switch between different cell states and are able to change from being less aggressive (“epithelial”) to being more aggressive (“mesenchymal”), and vice versa. By converting highly aggressive cancer cells to become less aggressive, physicians can prime tumors to respond better to chemotherapy, which works to eliminate cancer cells. This discovery has led to the launch of a three-year long human clinical trial, BEXMET (Bexarotene-induced Mesenchymal-Epithelial Transition), to investigate this unconventional approach to treating TNBC.
TNBC is more aggressive than other breast cancer sub-types, with limited treatment options and a poor prognosis. TNBC tests negative for estrogen receptor (ER), progesterone receptor (PR) and human epithelial growth factor receptor-2 (HER2), hence the reference to ‘triple-negative’ in its name. This also means that treatments targeting ER, PR and HER2 are not effective. For that reason, chemotherapy is still the mainstay standard treatment for TNBC.
The development of novel oncology drugs is costly, and affordability and accessibility can be a challenge. The concept tested by the NCCS, SGH and GIS team involves altering cancer cell states so that they are more susceptible to currently available chemotherapy. This may be a cost-effective way to treat TNBC, with the potential to treat a wider range of other cancers.
The team began by studying breast cancer tissue from NCCS and SGH patients in 2017 to understand pathways that control the behavior of cancer cells, in terms of their ability to invade and spread. Leveraging highly advanced genome sequencing and functional genomic capabilities at GIS, the research found that Bexarotene—belonging to a class of drugs known as retinoids—is able to convert the more aggressive “mesenchymal” cell state to a less aggressive “epithelial” cell state. This biological process is also termed mesenchymal-to-epithelial transition (MET). This is the first time that Bexarotene has been employed to facilitate the MET process in preclinical breast cancer work.

These findings were published in the journal Science Advances on 7 October 2021. The study was led by co-senior author, Dr. Tam Wai Leong, Associate Director and Group Leader of the Laboratory of Translational Cancer Biology at GIS.
“Cancer cells are crafty and have ways to evade treatment, sometimes through taking on this drug-resistant ‘mesenchymal’ cell state. Instead of tackling the tumors conventionally with direct administration of chemotherapy, the solution may be to first coax them into a less aggressive state before chemotherapy is given. This is a departure from standard cancer treatment,” said Dr. Tam. “Taming the behavior of such malignant cells prior to their ablation may work better and result in more durable clinical responses.”
In preclinical tests performed in animal models, Bexarotene changed TNBC cell states from mesenchymal to epithelial, rendering the TNBC cells more susceptible to conventional chemotherapy, which resulted in longer lasting responses that kept cancer relapse at bay.

These laboratory findings were directly translated to the human setting with the clinical trial, BEXMET. The trial aims to validate Bexarotene-induced TNBC cell state changes that were observed pre-clinically, and assess the tolerability and efficacy of the Bexarotene-Capecitabine chemotherapy combination.
Source: Read Full Article