A recent study published in the journal Public Library of Science (PLOS) ONE presented the T cell and humoral immune responses following severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccination and infection against the SARS-CoV-2 original and mutant strains.
 Study: SARS-CoV2 wild type and mutant specific humoral and T cell immunity is superior after vaccination than after natural infection. Image Credit: fusebulb / Shutterstock
Study: SARS-CoV2 wild type and mutant specific humoral and T cell immunity is superior after vaccination than after natural infection. Image Credit: fusebulb / Shutterstock
Background
Following the emergence of SARS-CoV-2 in late December 2019, the coronavirus disease 2019 (COVID-19) pandemic has affected global health systems. Shortly after SARS-CoV-2 emergence, numerous COVID-19 vaccines were developed centered on the SARS-CoV-2 original (Wuhan) strain spike (S) sequence.
SARS-CoV-2, like other ribonucleic acid (RNA) viruses, is vulnerable to mutational changes over time. As a result of the widespread dissemination of the COVID-19 pandemic, adaptive changes are more likely to emerge, potentially leading to selective viral benefits such as improved attachment to human cells or immunological escape from neutralizing antibodies. Mutations in the SARS-CoV-2 S receptor-binding domain (RBD) are concerning since the virus gains host cell entry through this region. Furthermore, the altered amino acid residues in the mutants can affect SARS-CoV-2 neutralization by vaccine or natural infection-induced antibody responses.
About the study
The present study aimed to discover more about immune responses to naturally occurring SARS-CoV-2 infections versus COVID-19 vaccination for the most severe mutant virus types. The researchers evaluated long (up to one year)- and short (<2 months)-term antibody and T cell responses in blood samples from completely COVID-19 vaccinated subjects and priorly SARS-CoV-2-positive tested individuals to the viral original and mutant sequences, with specific attention to the SARS-CoV-2 Delta (B.1.617.2) variant. Individuals were deemed fully COVID-19 vaccinated if there had been two weeks since their last shot of either a messenger RNA (mRNA)-based (mRNA-1273, BNT162b2) or vector-based (ChAdOx1 nCoV-19) vaccine.
The scientists assessed the anti-SARS-CoV-2 S and anti-nucleocapsid (N) protein antibody titers in the participants. The team determined the antibody-mediated average SARS-CoV-2 neutralization as the hindrance of angiotensin-converting enzyme 2 (ACE2) adherence to wild type (wt) and Delta RBD. Flow cytometric intracellular cytokine staining was used to evaluate SARS-CoV-2 S protein-specific CD4+ T cell responses following stimulation with peptide pools from the SARS-CoV-2 Delta, Gamma, Beta, Alpha, or wt mutant S proteins.
Results
The study results demonstrated that considering serum antibody binding to wild type (wt) and mutant virus proteins, all individuals vaccinated against SARS-CoV-2 had significant humoral immune responses. High anti-SARS-CoV-2 S protein RBD antibody titers were present in 23 COVID-19 vaccinees. Antibody-facilitated average SARS-CoV-2 neutralization was 2.2 times lower in the RBD of the SARS-CoV-2 Delta mutant than in the wt.
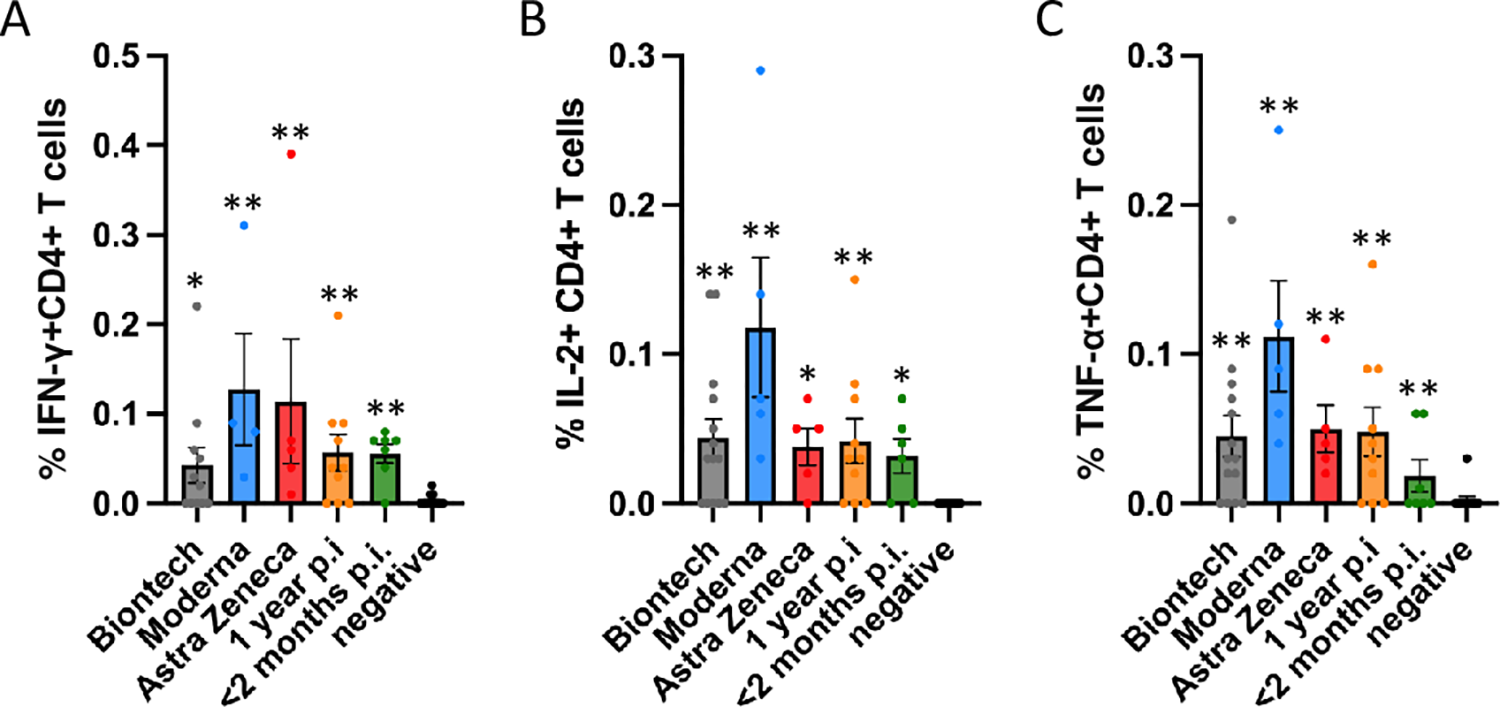 Antigen-specific CD4+ T cell responses elicited by the Miltenyi wt S protein peptide pool after vaccination with BioNtech (grey), Moderna (blue) or AstraZeneca (red), or one year (orange) or < 2 months (dark green) after naturally occurring infection with SARS-CoV2. In comparison, samples of healthy control subjects, who tested negative for SARS-CoV2-antibodies, are shown on the right of each panel. The bar graphs show frequencies of (A) interferon-γ (IFN-γ), (B) interleukin-2 (IL-2)- and (C) tumor necrosis factor-α (TNF-α)-positive CD4+ T cells. The figure shows results of n = 13 independent individuals after vaccination with BioNtech, n = 5 Moderna, n = 5 AstraZeneca, and n = 10 independent individuals one year and n = 7 subjects < 2 months after natural infection with standard errors of the mean (SEM). For comparison, 13 negative healthy controls were included. Significance levels were tested by Kruskal-Wallis test for non-parametric values. *p < 0.05, **p < 0.01 vs. healthy controls.
Antigen-specific CD4+ T cell responses elicited by the Miltenyi wt S protein peptide pool after vaccination with BioNtech (grey), Moderna (blue) or AstraZeneca (red), or one year (orange) or < 2 months (dark green) after naturally occurring infection with SARS-CoV2. In comparison, samples of healthy control subjects, who tested negative for SARS-CoV2-antibodies, are shown on the right of each panel. The bar graphs show frequencies of (A) interferon-γ (IFN-γ), (B) interleukin-2 (IL-2)- and (C) tumor necrosis factor-α (TNF-α)-positive CD4+ T cells. The figure shows results of n = 13 independent individuals after vaccination with BioNtech, n = 5 Moderna, n = 5 AstraZeneca, and n = 10 independent individuals one year and n = 7 subjects < 2 months after natural infection with standard errors of the mean (SEM). For comparison, 13 negative healthy controls were included. Significance levels were tested by Kruskal-Wallis test for non-parametric values. *p < 0.05, **p < 0.01 vs. healthy controls.
In more than 90% of COVID-19 vaccinees, SARS-CoV-2 neutralizing titers (NT50) remained considerably above the level correlated with immune protection in recent vaccination studies. SARS-CoV-2 neutralization ability was declined in many participants after COVID-19 and those who had received one dose of the vaccination. One year after natural SARS-CoV-2 infection, mean specific antibody titers were lower than after COVID-19 vaccination, indicated by the 1.65-fold lower ACE2 binding to the Delta mutant RBD versus the wt strain.
Many SARS-CoV-2 strains showed reduced cross-neutralization, which might affect COVID-19 vaccination effectiveness. The authors observed that Omicron RBD binding was decreased compared to the Delta variant.
The researchers discovered robust CD4+ T cell responses to SARS-CoV-2 mutant (Delta and Gamma) or wt S proteins. However, no particular CD8+ T cell response was seen, which might be because the 15-meric peptide pool used was insufficient to excite CD8+ T cells. Further, the authors found no drastic variation between the two-dose vaccinated study volunteers in cytokine production of tumor necrosis factor α (TNF-α), interleukin 2 (IL-2), or interferon γ (IFN-γ). Compared to vaccinated subjects, T cell responses to SARS-CoV-2 mutant or wt S proteins were substantially lower following SARS-CoV-2 infection.
Conclusions
According to the authors, this was the first work that carefully compared inhibition experiments that utilized labeled SARS-CoV-2 mutant versus wt RBD and ACE2 coated plates with those in which ACE2 was labeled and put in solution to mutant against wt RBD-coated plates.
The study findings depicted that the SARS-CoV-2 Delta mutant had lower antibody neutralization than the viral wt strain, as demonstrated in the new inhibitory assessment with a finger-prick blood drop. Strong CD4 T cell responses were found against SARS-CoV-2 mutant and wt strains, including the Delta (B.1.617.2) variant, in fully vaccinated subjects. However, CD4 T cell responses were somewhat weaker one year after natural SARS-CoV-2 infection.
Overall, these data imply that immunological responses following SARS-CoV-2 vaccination were more significant than those following naturally occurring COVID-19, highlighting the necessity for the vaccine to combat the SARS-CoV-2 pandemic. Furthermore, the present findings showed that using a combination of rapid production of recombinant proteins in mammalian cell systems and adoptive T cell assays, immunological responses to SARS-CoV-2 variants could be investigated within three months of their emergence.
Immune reactivity to future SARS-CoV-2 variants of concern and present viral mutants will allow vaccination methods to be adjusted to give population protection against new SARS-CoV-2 lineages of concern and to track the novel mutants spread. In light of the worldwide mutant spread, these findings suggest that additional COVID-19 vaccination should be undertaken following spontaneous SARS-CoV-2 infection. Moreover, the present paper describes a complementary diagnostic panel that could measure immunological reactivity to COVID-19 vaccines.
- Richardson JR, Götz R, Mayr V, Lohse MJ, Holthoff HP, et al. (2022) SARS-CoV2 wild type and mutant specific humoral and T cell immunity is superior after vaccination than after natural infection, PLOS ONE 17(4): e0266701, DOI: https://doi.org/10.1371/journal.pone.0266701, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0266701
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Amino Acid, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Antigen, Blood, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, covid-19, Cytokine, Diagnostic, Enzyme, Global Health, Health Systems, immunity, Interferon, Interleukin, Interleukin-2, Intracellular, Necrosis, Omicron, Pandemic, Protein, Receptor, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, T-Cell, Tumor, Tumor Necrosis Factor, Vaccine, Virus

Written by
Shanet Susan Alex
Shanet Susan Alex, a medical writer, based in Kerala, India, is a Doctor of Pharmacy graduate from Kerala University of Health Sciences. Her academic background is in clinical pharmacy and research, and she is passionate about medical writing. Shanet has published papers in the International Journal of Medical Science and Current Research (IJMSCR), the International Journal of Pharmacy (IJP), and the International Journal of Medical Science and Applied Research (IJMSAR). Apart from work, she enjoys listening to music and watching movies.
Source: Read Full Article