An international research team led by the German University of Jena has now developed a promising approach to significantly reducing blood clotting on the heart valve material titanium.
Around 25,000 artificial heart valves are implanted in Germany per year because the original heart valve is damaged, for example, by an infection. The mechanical heart valves are made of titanium dioxide, among other materials, and last for many years. However, because blood tends to clot on contact with these material surfaces, there is a risk of blood clots forming on the surface of mechanical heart valves. This can become life-threatening if such blood clots break away from the materials. For this reason, most people with mechanical heart valves take medication throughout their lives to reduce blood clotting.
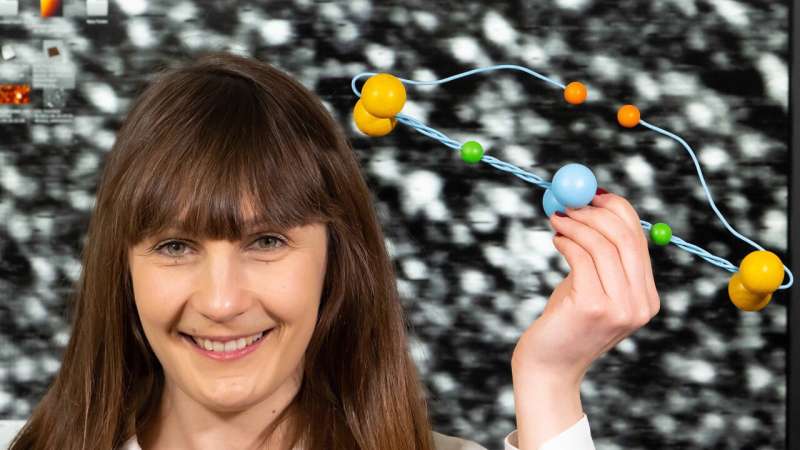
An international research team has now developed a promising approach to significantly reducing blood clotting on the heart valve material titanium. The results of the team from the Universities of Jena, Leipzig (both Germany) and Illinois Urbana-Champaign (U.S.), led by materials scientist Professor Klaus D. Jandt, have now been published in the journal Advanced Healthcare Materials. The journal also acknowledges the importance and potential of this discovery by featuring it on the cover of the current issue.
Platelet activity changes according to material coating
The researchers produced deposits of the blood protein fibrinogen on titanium dioxide with crystallographically differently oriented surfaces. The coated material surfaces then were exposed to blood platelets (thrombocytes), the activity of which, together with fibrinogen, plays a decisive role in the formation of blood clots. Significant differences in platelet activity were found on the material surfaces with different orientations.
“While the platelets are very active on (001) titanium oxide surfaces and thus promote blood clotting, we found the opposite effect on (110) surfaces,” says Ph.D. student Maja Struczynska. “The reason for this is the different behavior of fibrinogen on the material surfaces.”
“The mechanism for this effect is physical,” says Prof. Jandt. “Fibrinogen adopts a specific fold on the more hydrophobic (110) surface with low surface energy, which in turn limits the access of the primary amino acid sequences recognized by platelets, thus minimizing their adhesion.” Jandt sees enormous potential in the application of these materials to heart valves, as it should reduce the risk of blood clot formation and associated complications, and thus be of benefit to those affected.
More information:
Maja Struczyńska et al, How Crystallographic Orientation‐Induced Fibrinogen Conformation Affects Platelet Adhesion and Activation on TiO 2, Advanced Healthcare Materials (2023). DOI: 10.1002/adhm.202202508
Journal information:
Advanced Healthcare Materials
Source: Read Full Article