Researchers in Cuba have presented the results of phase 1 and phase 2 clinical trials of a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) recombinant spike protein vaccine (Abdala). The vaccine is found to be safe, well-tolerated, and induces substantial humoral immune responses against SARS-CoV-2 among adults 19 to 80 years of age.
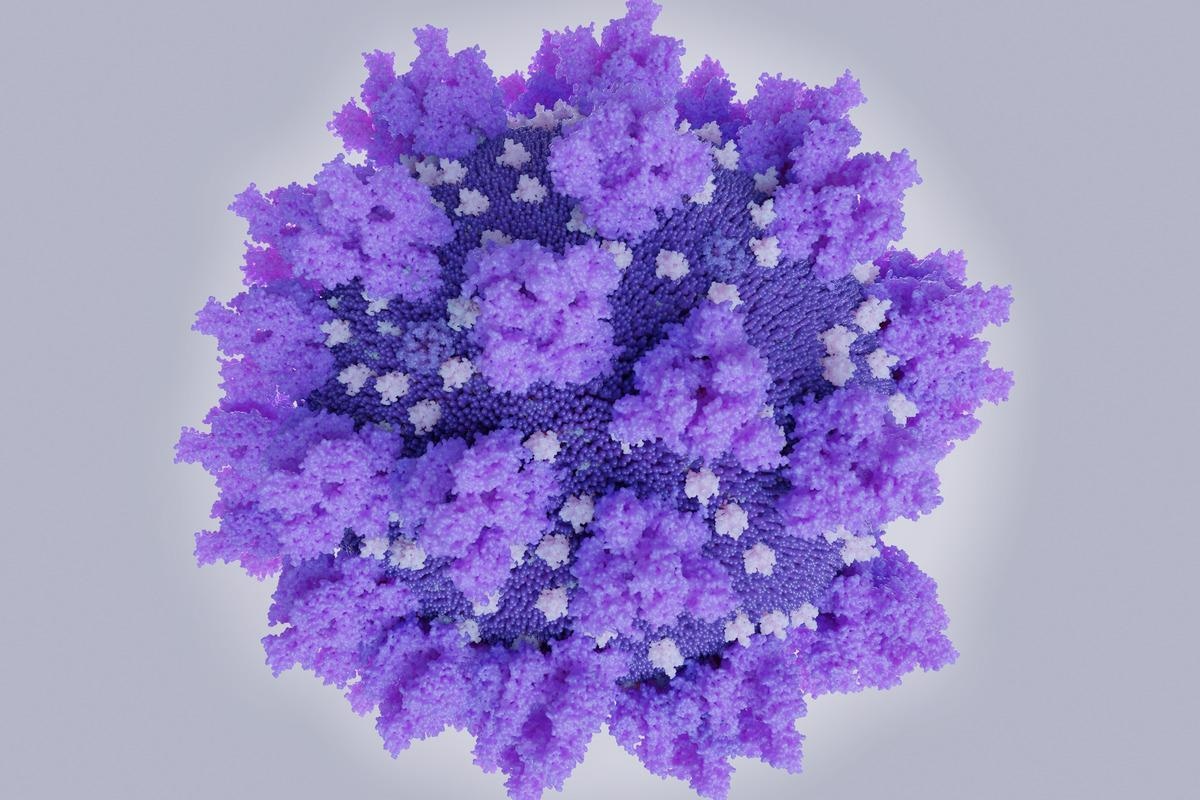 Study: Safety, tolerability, and immunogenicity of a SARS-CoV-2 recombinant spike protein vaccine: a randomised, double-blind, placebo-controlled, phase 1-2 clinical trial (ABDALA Study). Image Credit: Juan Gaertner/Shutterstock
Study: Safety, tolerability, and immunogenicity of a SARS-CoV-2 recombinant spike protein vaccine: a randomised, double-blind, placebo-controlled, phase 1-2 clinical trial (ABDALA Study). Image Credit: Juan Gaertner/Shutterstock
The study was meant to evaluate the safety, tolerability, and immunogenicity of the newly developed vaccine administered intramuscularly in different strengths and vaccination schedules.
A pre-print version of the research paper is available on the medRxiv* server while the article undergoes peer review.
Background
The coronavirus disease 2019 (COVID-19) global pandemic continues to devastate the world even after two years of its initial origin in December 2019 from Wuhan, China. Obtaining safe and effective vaccines and implementing them with broad global coverage is the fastest and safest strategy to manage the consequences of this pandemic. Thus, clinical trials on multiple prophylactic vaccine candidates with accelerated designs are currently being carried out worldwide.
The Centre for Genetic Engineering and Biotechnology, Havana (Cuba), developed a vaccine candidate named Abdala, based on a recombinant receptor-binding domain (RBD) subunit of the spike protein produced in Pichia pastoris yeast and adjuvanted to alumina.
A randomized, adaptive, double-blind, placebo-controlled, phase 1-2 clinical trial was conducted to assess this vaccine candidate's safety and immunogenicity profile.
Phase 1 Abdala study
A total of 132 subjects were included in the phase 1 trial, randomly distributed into two vaccination schedules (0-14-28 and 0-28-56 days) and three study groups for each schedule (placebo and two RBD strengths: 25μg and 50μg).
Blood samples were collected at day 0, before applying the first dose (baseline), at days 42 and 56 for the schedule 0-14-28 days, and at days 56 and 70 for the schedule 0-28-56 days to determine the level of anti-RBD IgG and neutralizing antibodies. Geometric mean titers (GMT) of anti-RBD IgG and neutralizing antibodies and the percentage of inhibition of RBD-ACE-2 binding were also determined.
The product was well tolerated. Adverse events were minimal, most resolved spontaneously in the first 24-48 hours without medication, and there were no withdrawals for this cause.
The primary immunogenicity outcome was the seroconversion rate of the IgG RBD-binding antibodies and was defined as at least a four-fold increase of antibody titers over the baseline.
In phase 1, none of the participants in the placebo groups were seroconverted, whereas high seroconversion rates were obtained for both strengths of RBD/vaccination schedules.
At day 56 (28 days after the third dose of the short vaccination schedule, 0-14-28 days), seroconversion of anti-RBD IgG was seen in 95.2% of the participants (20/21) for the 50μg group and 81% of the participants (17/21) for the 25μg group, whereas neutralizing antibodies to SARS-CoV-2 were seen in 80% of the participants (8/10) for the 50μg group and 94.7% of the participants (18/19) for the 25μg group.
For the long schedule, at day 70 (14 days after the third dose), seroconversion of anti- RBD IgG was seen in 100% of the participants (21/21) for the 50μg group and 94.7% of the participants (18/19) for the 25μg group, whereas neutralizing antibodies to SARS-CoV-2 were seen in 95 % of the participants (19/20) for the 50μg group and 93.8% of the participants (15/16) for the 25μg group.
Phase 2 Abdala study
After an interim analysis of the phase 1 trial results and given the complex epidemiological situation resulting from the COVID-19 pandemic where it was necessary to immunize people in the shortest possible time, the team strategically decided to continue towards phase 2 of the trial with the three study groups of the short vaccination schedule (0-14-28 days).
Therefore, phase 2 included 660 new subjects, to which were added the 66 subjects evaluated in a similar vaccination scheme during the first trial (726 subjects in total; 242 in each study group).
In phase 2, only the short scheme (0-14-28 days) was evaluated during the interim analysis. Blood samples were collected at day 0, day 42, and day 56 (14 and 28 days after the third dose).
On day 56, seroconversion of anti-RBD IgG was seen in 89.2% of the participants (214/240) for the 50μg group, 77.7% of the participants (185/238) for the 25μg group, and 4.6% in the placebo group (11/239); whereas neutralizing antibodies to SARS-CoV-2 were seen in 97.3% of the participants (146/150) for the 50μg group and 95.1% of the participants (58/61) for the 25μg group.
Three dose schedule of Abdala vaccine induces high immune responses in adults 19-80 years old
The safety and immunogenicity analyses demonstrated that three doses of Abdala at different strengths and different immunization schedules were safe and induced high immune responses in adults 19 to 80 years of age, including neutralizing antibodies correlated with the anti-RBD IgG response.
The incidence of adverse reactions in the 25μg and 50μg groups were similar, indicating no dose-related safety issue. The adverse reactions reported were minimal.
The team highlights that although most of the COVID-19 vaccines already in use are administered mainly in schedules of two doses and the three-dose schedule can be thought of as complicated and time-consuming, the short immunization schedule proposed in this trial (0-14-28 days) would allow for only one month the vaccination regimen to be completed with a good immunogenic profile. Potentially a third dose instead of only two doses in this short time would be more favorable.
Phase 2 results were consistent with those obtained previously in phase 1 trial. They confirmed the favorable immunogenic profile of the Abdala vaccine with better results and risk-benefit ratio for the 50μg dose group.
The vaccine's better immunological performance was obtained in the age group 19-54 years compared to the older individuals aged 55-80 years. Age is considered an important factor influencing the immune response to vaccines, and this effect has been found for several vaccines where older people have lower antibody levels. Nevertheless, more than 80% of the subjects were seroconverted in the study. Other COVID-19 vaccines have shown lower responses in older individuals when compared with the youngest ages.
"The level of in vitro antibody response does not necessarily correlate with health outcomes, i.e., seroconversion does not mean complete protection against a disease, and non-seroconversion is not necessarily associated with susceptibility, not to mention that antibody levels decline over time, but seronegative individuals may still be protected through other immune mechanisms, as shown, for example, after hepatitis B vaccination" the team highlights.
Pearson's linear correlation analyses found positive and highly significant correlations between different immunogenicity variables, indicating that the immune response for the vaccine is potent both in quantity and the quality of the antibodies elicited.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Hernandez-Bernal F., et al. (2021) Safety, tolerability, and immunogenicity of a SARS-CoV-2 recombinant spike protein vaccine: a randomised, double-blind, placebo-controlled, phase 1-2 clinical trial (ABDALA Study). medRxiv. doi: https://doi.org/10.1101/2021.11.30.21267047, https://www.medrxiv.org/content/10.1101/2021.11.30.21267047v2
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antibodies, Antibody, Biotechnology, Blood, Clinical Trial, Coronavirus, Coronavirus Disease COVID-19, Genetic, Genetic Engineering, Hepatitis, Hepatitis B, Immune Response, Immunization, in vitro, Pandemic, Placebo, Protein, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Vaccine, Yeast

Written by
Namita Mitra
After earning a bachelor’s degree in Veterinary Sciences and Animal Health (BVSc) in 2013, Namita went on to pursue a Master of Veterinary Microbiology from GADVASU, India. Her Master’s research on the molecular and histopathological diagnosis of avian oncogenic viruses in poultry brought her two national awards. In 2013, she was conferred a doctoral degree in Animal Biotechnology that concluded with her research findings on expression profiling of apoptosis-associated genes in canine mammary tumors. Right after her graduation, Namita worked as Assistant Professor of Animal Biotechnology and taught the courses of Animal Cell Culture, Animal Genetic Engineering, and Molecular Immunology.
Source: Read Full Article