In the early stages of the COVID-19 pandemic, the disease was recognized as a respiratory virus. Research is showing that the SARS-CoV-2 virus is causing more significant cardiac issues than initially thought.
“We are finding that COVID-19 can cause direct damage to the heart,” says Dr. Leslie Cooper, chair of the Department of Cardiology at Mayo Clinic.
Although individuals with cardiovascular disease are at increased risk for more severe complications from COVID-19, Dr. Cooper says any person infected with the virus may be at risk for cardiac involvement.
“COVID can affect the heart indirectly through inflammatory cells that circulate in your blood that can go into the heart and by damaging heart muscle cells as well,” he says.
Of late, COVID-related myocarditis, or inflammation of the heart muscle, is the condition that is causing growing concern. Myocarditis can cause significant heart damage and rarely sudden cardiac death if it’s left untreated. “Myocarditis and other forms of heart injury can affect younger individuals, such as athletes.”
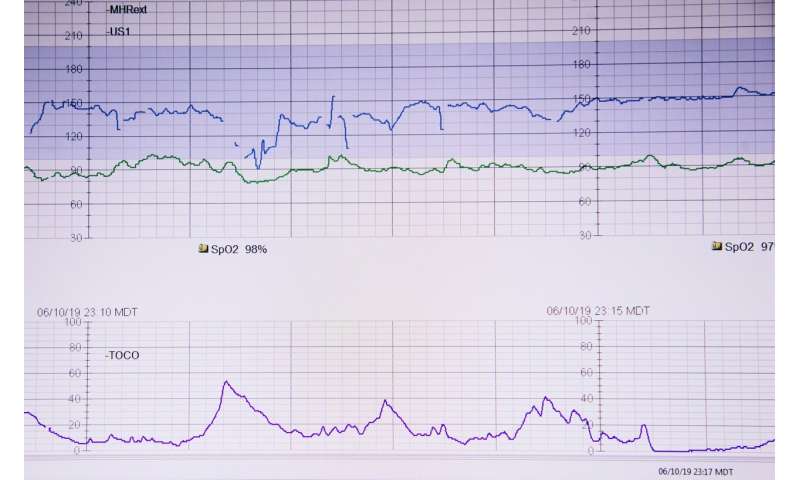
Though not everyone needs to be tested, Dr. Cooper says patients suspected to have COVID-19 related cardiac injury would undergo tests, including a troponin blood test, which can reveal damaged heart muscles cells, and an electrocardiogram or EKG, which can show involvement of the conduction system of the heart or damage of the heart muscle. Finally, in those people who have symptoms of heart involvement and show abnormality in the blood test or EKG, an echocardiogram or other advanced imaging may be obtained.
As the COVID-19 pandemic continues, Dr. Cooper adds that there is intense research around the long-term effects of the virus on the heart.
“There have been several reports where people are clinically better but there’s still imaging evidence of some cardiac injury, and we do not know yet the clinical significance – meaning a risk of arrhythmias or future heart failure – from these imaging findings,” he says. “It will be important to follow patients prospectively to determine what the actual risk is.”
Dr. Cooper adds that we will likely see an increase in testing as outcomes research continues.
He also notes that it is important for people to be aware of their symptoms since cardiac issues may not be obvious. He advises that anyone, whether they have COVID-19 or not, be aware of new chest pain, trouble breathing and shortness of breath.
“If you develop new chest pain, particularly if it’s with exertion or moving to different positions, or new trouble breathing, shortness of breathe at rest or with activities, those are reasons you should go and get an evaluation that could include cardiac studies,” says Dr. Cooper.
Source: Read Full Article