A new COVID variant has recently been detected in several countries including the UK, US, India, Australia and Germany.
Called BA.2.75, it’s a subvariant of omicron. You might have also heard it called “Centaurus,” the name of a constellation and given to BA.2.75 by a Twitter user.
The World Health Organization has classified BA.2.75 as a variant of interest, rather than a variant of concern. This means it’s being monitored but there’s not yet evidence it will cause problems.
The numbers of BA.2.75 infections are still relatively low. Most infections in the UK remain driven by the omicron subvariants BA.4 and BA.5. BA.5 in particular is similarly dominant in other countries where BA.2.75 has been detected.
However, BA.2.75 is becoming more common in India (where it was first detected, back in May), suggesting it has advantages relative to current circulating variants. Some have noted that BA.2.75 is spreading in regions of India where it doesn’t have to compete with BA.5, but rather with the variant it evolved from, BA.2.
That said, some data from India indicates that BA.2.75 may have already peaked. And importantly, there hasn’t been a big increase in hospitalizations or deaths in India from BA.2.75.
Given this, BA.2.75 has quickly gained an additional nickname: a “scariant”.
Why are we still seeing new variants?
As most of the global population has now either been vaccinated, infected, or both, variants which can infect people despite their immunity will have an advantage. So SARS-CoV-2 (the virus that causes COVID) is constantly evolving to gain this advantage.
New variants which have mutations that evade our immunity will replicate and spread, leading to waves of infections. We’ve seen this most recently with BA.4 and BA.5.
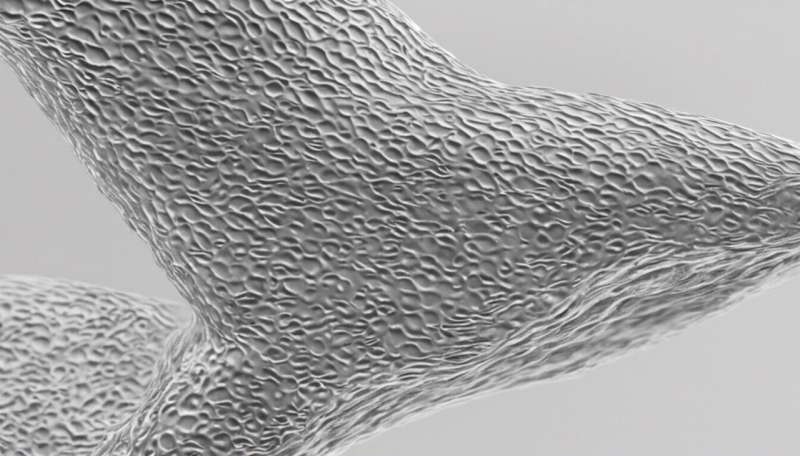
The memory immune system recognizes infections based on molecular structures of viruses and other pathogens. Mutations change the molecular structure of each SARS-CoV-2 variant slightly, making it more difficult for our immune system to recognize and respond to the virus. This is often called “immune evasion.”
The concern around BA.2.75 is that is has picked up a number of mutations, which might indicate that this variant can evade immunity. But there’s no good evidence at this stage that BA.2.75 can evade the immune system in a significant way.
Most of BA.2.75 is structurally the same as omicron and the original Wuhan variant. Although BA.2.75 has picked up a few mutations, it isn’t fundamentally a different virus.
The memory immune system will still act against BA.2.75, which is what we’ve seen with omicron. This immunity might not be enough to stop reinfection, but should reduce the severity of a BA.2.75 infection.
While there are concerns BA.2.75 could spread more quickly than other variants, we don’t have any clear evidence on this yet. It seems to have shown an increase which has leveled off or even dropped relative to a few weeks ago. If this is the case there’s a chance it might even fizzle out in another few weeks.
But, if BA.2.75 does have some immune evasion properties, it could cause another wave through the UK and elsewhere. Still, this would likely spike and then fizzle out like alpha, delta and omicron BA.1.
Improving vaccines could be our best shot
Thanks to vaccination, if we did face a BA.2.75 wave, we wouldn’t expect the level of deaths and hospitalizations seen earlier in the pandemic. But we know large numbers of cases can still cause significant disruption. And importantly, the constant wave of new variants is still a deadly threat to people who are vulnerable. So how do we overcome this?
One solution could be universal COVID vaccines, which would work against any COVID variants. The aim of a universal vaccine is to induce immunity against a very wide range of molecular structures. It’s akin to fishing with a wider net, making it harder for the fish to swim out of the way.
A pan-coronavirus vaccine is a similar concept but would likely try to induce immunity against the molecular structures common to all coronaviruses. As well providing immunity against new SARS-CoV-2 variants, a pan-coronavirus vaccine might also confer immunity against the next coronavirus pandemic. Some of these vaccines look set to move into clinical trials in the next few years.
A second solution may be to produce vaccines which induce better immunity in the respiratory system. These largely involve vaccines given through your nose, training the immune system to make more antibodies in the mucus of the nose and throat.
This type of immunity might help stop SARS-CoV-2 infecting and replicating at the point of entry into our cells, which could slow down the rate at which new variants have the opportunity to emerge. At least 12 of these intranasal vaccines are in clinical trials.
Source: Read Full Article