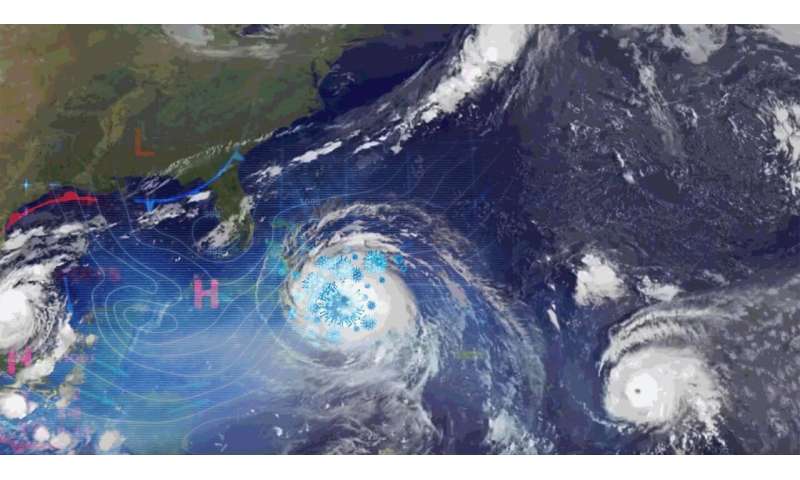
Princeton disease ecologist C. Jessica Metcalf and Harvard physician and epidemiologist Michael Mina say that predicting disease could become as commonplace as predicting the weather. The Global Immunological Observatory, like a weather center forecasting a tornado or hurricane, would alert the world, earlier than ever before, to dangerous emerging pathogens like SARS-CoV-2.
In late October 1859, one of the century’s most devastating storms struck the British Isles. Winds, estimated at over 100 mph, howled across the Irish Sea. The storm destroyed 133 ships and caused at least 800 deaths, more than half on the Royal Charter, a steam clipper built to handle the increased gold rush traffic to Australia.
Despite early signs of the impending storm, the captain pushed forward instead of seeking shelter. He was caught off guard by a gale, which overpowered the ship and sent it careening into the rocky shoreline. Any warning of the storm’s strength would have prevented the tragedy.
Storm prediction was thought to be impossible at the time, even considered sacrilegious by some. But in the aftermath of the Royal Charter disaster, one scientist was convinced it could have been averted.
Robert FitzRoy, best known as Charles Darwin’s salty captain aboard the HMS Beagle, was the head of a new program to catalog weather observations made by ships at sea. Using his growing knowledge of weather patterns and his arsenal of charts, barometers and thermometers, FitzRoy demonstrated that he could have predicted the storm, allowing time for ships to change course. Weather forecasting—a term FitzRoy coined—could save countless lives.
FitzRoy’s early methods pale in comparison to the global, unified effort that now produces our hourly weather forecasts. Thousands of buoys, distributed across the world’s oceans, measure sea-surface temperatures. Weather stations and satellites feed data into complex computer models. Anyone with a computer or smartphone can gain a (mostly) accurate picture of current and future weather, anywhere in the world. We take for granted our ability to check the forecast.
Today, we find ourselves in a different kind of storm. Like the captain and crew of the Royal Charter, the world has been caught off guard—this time, by a devastating illness.
COVID-19 isn’t the first global pandemic, and it won’t be the last. The emergence of disease, from the Black Death to the novel coronavirus, is as unpredictable as the weather was in past centuries. Now, scientists at Princeton, in collaboration with others, are working toward a future where pandemics are predicted, prepared for and—in some cases—prevented.
“If this pandemic has made one thing obvious, it’s that the health of any of us is the health of all of us,” said C. Jessica Metcalf, a disease ecologist at Princeton University.
Metcalf, together with epidemiologists and immunologists from Princeton, Harvard University, the Wellcome Trust and the National Institutes of Health, pitched an idea for a new and revolutionary approach to global health—a way to make predicting disease as commonplace as predicting the weather.
They call it a Global Immunological Observatory, or GIO. Like a weather center, it would monitor the world’s health by compiling data in a systematic and cohesive way. And, like a weather center forecasting a tornado or hurricane, a GIO could alert the world, earlier than ever before, to a dangerous emerging pathogen like SARS-CoV-2.
Had such an approach been in place, countries could have initiated a more cohesive and global response early in the coronavirus pandemic, potentially saving countless lives.
“We’re going to do our damnedest to try and make it happen, because it would be crazy not to,” said Metcalf, associate professor of ecology and evolutionary biology and public affairs in Princeton’s School of Public and International Affairs.
What’s today’s health forecast?
It’s December. You’re packing for a trip home for the holidays. Your smartphone informs you to expect subzero temperatures in Minneapolis, so you pack your heavy winter coat. You scroll down and learn your home zip code is experiencing a particularly high caseload of seasonal flu. You add a few masks to your bag, just in case.
“Every day, we have parents looking at their kids and saying, “You have a runny nose, I wonder what it is? Maybe it’s the flu,” said Michael Mina, a physician and assistant professor of epidemiology at Harvard T.H. Chan School of Public Health. “We go to the doctor. But most of the world doesn’t have that as an option.”
A GIO would provide parents with a way to check local disease conditions. Maybe the parent learns there is a local outbreak of the common cold, not the flu, and so skips the trip to the doctor. Staying home saves time, resources and prevents spreading the disease further.
Metcalf and Mina were the two leading authors of an article pitching the GIO in the June 2020 edition of the journal eLife. The other co-authors were leading immunologists and disease ecologists: Adrian McDermott and Daniel Douek of the Vaccine Research Center at the National Institute of Allergy and Infectious Diseases; Jeremy Farrar, director of the Wellcome Trust; and Bryan Grenfell, the Kathryn Briger and Sarah Fenton Professor of Ecology and Evolutionary Biology and Public Affairs.
Mina, who prior to joining Harvard conducted postdoctoral research at Princeton in infectious disease dynamics with Grenfell, envisions the GIO as an open and accessible resource for everyone, providing immunity data by zip code.
But its usefulness in “peacetime”—what epidemiologists call the time between pandemics—is just a bonus. Its true power is detecting novel pathogens and acting as an early warning system.
“Had we had this running, we would have definitely been able to detect SARS-CoV-2,” Mina said.
With the earliest reports out of China, scientists would have been on high alert for strange signals in the stream of immunity data pouring into the GIO. They would have been able to detect a unique pattern emerging across the regions hit early by the pandemic—like New York, Washington and the San Francisco Bay Area. The first detection of those signals would have given Gov. Andrew Cuomo of New York the data-driven firepower to shutdown New York City a month earlier, Mina said.
“And that would have saved tens of thousands of lives,” he said.
A GIO would require an unprecedented level of collaboration between scientists and doctors, governments and citizens across the planet. And it would require blood.
“I think of the body as a constantly recording pathogen-detection device,” Mina said. “All we have to do is tap into the hard drives, which are the plasma cells and antibodies, to better understand what’s happening in our environment.”
Blood would provide the data that would drive the observatory. Antibodies, the y-shaped proteins responsible for detecting and neutralizing invaders, are found in our blood serum. They’re produced in response to infections, but each antibody can bind only to a specific pathogen.
The types and quantities of antibodies contained in our serum reflect our immune system’s past and present battles—a catalog of pathogens it has encountered, whether through infection or vaccine.
Until recently, most blood-serum tests detected antibodies for a single pathogen at a time. But recent breakthroughs have expanded that capability enormously. One example, a method developed at Harvard Medical School in 2015 called VirScan, can detect over 1,000 pathogens, including all of the more than 200 known viruses to infect humans, from a single drop of blood.
Using drops of blood collected from people spanning the globe, methods like VirScan could quickly paint a picture of humanity’s collective immune system. The more diverse that blood, the better resolution that picture will have.
“We just want to throw everything at it,” Metcalf said. “A lot of the work will be interpreting what we see.”
There are already robust methods for collecting blood serum at large scales—think of existing blood banks, supported by individual donations. For people who opt to contribute, they could learn about their own immunity and to which diseases they might be susceptible.
Once data from enough individuals is amassed, scientists could glean important insights about the threats facing humanity’s immune system. What demographics are hardest hit by the seasonal flu in Taiwan? What virus is responsible for this year’s cold outbreak in North Dakota?
The GIO concept is in a development phase, somewhere between idea and reality. Mina is pursuing the funding and construction of a flagship lab in Boston. Its first project will begin through a partnership with a company that has plasma donation sites across the United States.
By processing tens of thousands of samples, donated by people across the United States, the GIO’s first project will be an example, in miniature, of its global potential.
“We’re operating on the ‘build it and they will come’ logic,” Metcalf said.
The dark matter of epidemiology
For a given disease, a population can be categorized into three groups: those who are susceptible, those who became infected and those who have recovered. Most of what we know about COVID-19 is derived from active cases and mortality. But that describes only the middle category. The other two comprise what Metcalf and Mina call “the dark matter” of epidemiology. During a disease outbreak, a GIO would illuminate those poorly understood categories.
Susceptibility is difficult to assess, but it is critical for describing a disease’s progression through a population. As more people acquire immunity, either through infection or vaccination, the number of susceptible people shrinks. But identifying the populations that remain vulnerable can help prevent an unexpected resurgence of infections.
It indicates to public health experts if, and where, new outbreaks may occur.
This is precisely what the scientists in Metcalf’s lab aimed to investigate in Madagascar. Amy Winter, now a postdoctoral researcher at the Johns Hopkins Bloomberg School of Public Health, led an effort to investigate blood serum samples to explore the portion of Madagascar’s population that was susceptible to measles.
There were tens of thousands of annual cases of measles in the country until 2004, when widespread vaccinations successfully decreased the caseload to just a handful. Despite this successful mitigation, public health officials lacked data on the portion of the population that remained susceptible because they hadn’t been vaccinated.
The researchers thought the drop in cases might reflect a honeymoon period, where vaccinations significantly slowed the spread of the virus despite many susceptible individuals remaining in the population. To find out, Winter investigated existing blood serum samples that had been gathered a few years prior, to test if immunity was truly as widespread as the low caseload suggested.
The serum samples were far from ideal—they weren’t from a representative sample of the population, for instance. Metcalf said any classical epidemiologist would have been frustrated with the data. Yet, however imperfect, the data overwhelmingly revealed that many in the population lacked protection from the disease.
“Unequivocally, whatever we threw at it, we just kept seeing that there was an outbreak coming,” Metcalf said.
Unfortunately, their prediction was correct. A measles outbreak occurred in fall 2018, leading to an epidemic particularly among young children. Ongoing surveillance of blood serum antibodies would have described the extent of susceptible individuals long before the outbreak occurred. Vaccination efforts then could have targeted the demographics found to be susceptible, and yet another tragedy may have been averted.
Patchwork response in tatters
The COVID-19 pandemic has caused a confused and uneven response around the world. Some governments, particularly those on the frontlines of previous pandemics, effectively coordinated a response in the early days. Perhaps nowhere was the patchwork response exemplified, and its consequences felt more acutely, than in the United States. Despite suffering the world’s highest mortality, even simple interventions like mask mandates cause political divisions.
“Public health and infectious disease surveillance has been decreasingly funded for decades—people didn’t recognize the need,” Mina said. “It took one massive pandemic to bring our country to its knees. Having systems in place beforehand is just essential.”
As COVID-19 has displayed, many U.S. systems lack cohesion, from states disagreeing about lockdown rules like mask wearing to our lack of universal health care. Pioneering a GIO—a revolutionary effort to build cohesion in public health at a global scale—might be a tall order for a country that currently struggles to provide tests or basic health care for its citizens.
“The irony is not lost,” said Matthew Ferrari, an associate professor of biology at the Center for Infectious Disease Dynamics at Pennsylvania State University, who is not involved in the project. But Ferrari thinks this is exactly why the United States should lead the effort.
“We’ll benefit by creating equity within our borders as well as creating equity globally,” he said.
Although supportive, Ferrari has concerns about the GIO’s implementation. He points out that governments don’t always work well together, and people are bad at preparing for the future.
“There is real power in this kind of proactive investment,” he said. “What I’m skeptical of is the ability to put in place the global coordination for response.”
Knowing that a catastrophe is looming doesn’t always inspire people to change their behaviors. Consider climate change, for instance. Somewhere between optimism and pessimism, there exists the most likely human behavior: ambivalence.
“I think that history has shown that ambivalence rules, more often than not,” Ferrari said. The West African Ebola outbreak between 2014 and 2016 threatened a global pandemic. But despite efforts by scientists to implore governments to invest in preventing the next one, “here we are in 2020,” he said.
“The humanity of the people in West Africa should have been enough to keep us engaged last time,” he said.
Maybe this time will be different. Maybe with a disease threatening the world’s wealthiest nations, this catastrophe will encourage investment in the infrastructure to prepare for the next one.
If the GIO is successful at preventing pandemics, it could make the threat of disease seem less severe. In the case of COVID-19, some virus-deniers point to flattened curves as evidence that the virus isn’t as infectious or deadly as public health experts claim.
“It’s like putting your umbrella up and all the clouds go away,” Metcalf said.
The COVID-19 pandemic is a stark reminder that the ravages of disease aren’t only the harsh reality in far-off impoverished lands, she said. The complacency of wealthy nations demonstrates that immense resources alone cannot compensate for a lack of cohesive leadership and robust infrastructure.
A GIO would help the world prepare for the next great pandemic, but it can also chip away at the “background of tragedy,” to which Metcalf says we’ve all become desensitized.
“There’s a host of infections from which we should no longer be dying,” Metcalf said.
We can’t always avoid nasty weather, but forecasts can help us prepare. Some storms might only require an umbrella or a raincoat. Others might send us seeking shelter. A GIO can’t prevent the next disease from emerging, nor the next outbreak. But with the immense information it provides, accessible by all—public health officials, politicians and parents alike—the ability to prepare for our next encounter with an infectious disease could be at our fingertips.
Source: Read Full Article