An experimental drug restored brain synapses in two mouse models of Alzheimer’s disease, raising hopes that it could help revive cognitive function in human dementia patients, Yale University researchers report June 1 in the journal Science Translational Medicine.
While much research in Alzheimer’s has centered on reducing levels of beta-amyloid plaque in the brain that is a hallmark of the disease, recent studies have suggested that immune system response in the brain also plays a role in memory loss in patients.
Some scientists now believe that cognitive decline in Alzheimer’s patients results from a loss of synaptic connections between neurons caused by a steady accumulation of beta-amyloid protein in the brain which in turn unleashes a chronic immune system response to the intruder. The end stages of the disease lead to the death of neurons.
“The synapse loss triggered by beta-amyloid and inflammation is necessary to disrupt neural networks and cause cognitive decline seen in Alzheimer’s,” explained Stephen Strittmatter, the Vincent Coates Professor of Neurology and professor of neuroscience and co-corresponding author of the research at Yale. “Amyloid accumulation precedes inflammation and synapse loss, which is why people can have a buildup of amyloid for as much as a decade before they exhibit impaired memory and behavior.”
In recent years, Strittmatter, who is also director of the Kavli Institute for Neuroscience at Yale, and other scientists have focused on ways to halt synaptic loss in dementia patients without needing to remove amyloid from the brain. Biochemical discoveries led the Yale team to focus on the role played by cell receptor mGluR5, which helps regulate the signaling of neurotransmitter glutamate, in synaptic loss.
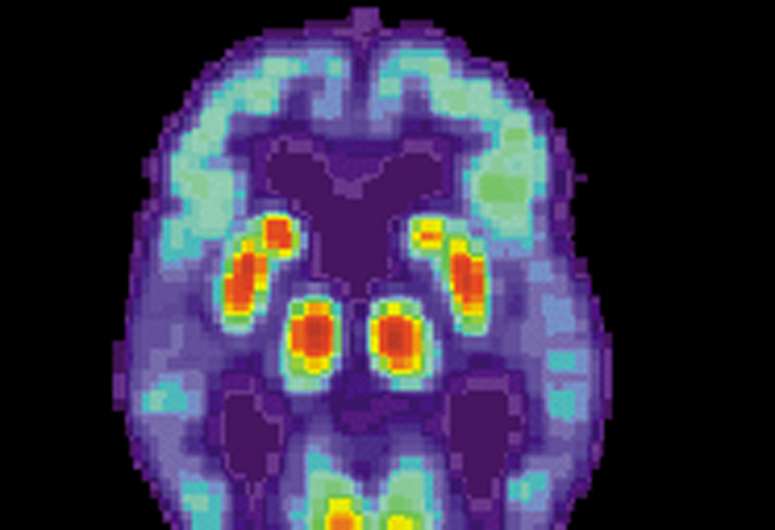
In the new study, PET imaging showed that synaptic connections were restored in mouse models of Alzheimer’s when they were given the drug known as Silent Allosteric Modulation or SAM (BMS-984923), which was developed by Bristol Myers Squibb as part of its effort to treat schizophrenia. The drug, which is administered orally, does not interfere with normal glutamate signaling in the brain, the researchers report. Critically, researchers also found that the drug restored normal gene expression patterns in the neurons of mice with models of Alzheimer’s disease.
Source: Read Full Article